During initial infection with HIV from anal or vaginal intercourse, a type of immune cell known as a dendritic cell (DC) is the first component of the immune system to encounter the virus at mucosal surfaces. Such surfaces protect the body from viruses and bacteria. DCs can migrate to lymph nodes and similar tissues, where contact with T cells may then play a key role in spreading the virus. This process, known as “trans infection,” occurs despite the fact that DCs themselves cannot be directly infected with HIV.
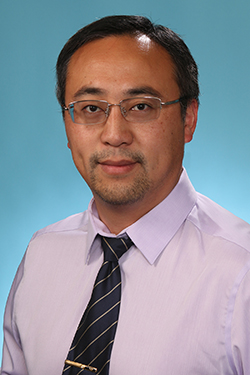
Dr. David Baltimore
In the January issue of the journal PLOS ONE, amfAR grantee and Nobel Prize laureate Dr. David Baltimore of Caltech in Pasadena, CA, with colleagues from the University of California, Los Angeles, the Max Planck Institute for Infection Biology in Berlin, and the Africa Health Research Institute in Durban, South Africa, examines this process in the test tube.
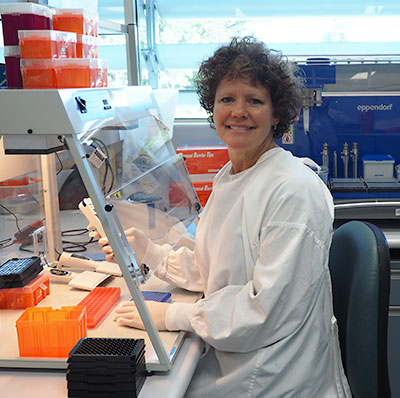
The investigators found that DCs can transmit HIV to T cells by direct contact despite the presence of two very potent anti-HIV drugs: the reverse transcriptase inhibitor tenofovir and the integrase inhibitor raltegravir. This was dependent on the number of DCs contacting a T cell and the amount of virus present in the body.
Researchers also discovered that DCs may increase the probability of establishing an HIV infection not only by transporting the virus, but also by amplifying the number of cells it can infect. DCs also reduce the anti-HIV potency of drugs. The latter is of particular concern in lymph nodes, which may have lower drug levels than in the blood and other tissues. It also has implications for HIV cure strategies.
The authors conclude: “Transmission of HIV by DCs in trans may have important implications for viral persistence in vivo in environments where residual replication may persist in the face of antiretroviral therapy.”
Dr. Laurence is amfAR’s senior scientific consultant.