Dr. Amy Chung
Researchers have long focused on natural killer (NK) cells as the principal cells of the immune system that receive a signal via antibodies to kill HIV-infected cells. In the May issue of the Journal of Immunological Methods, amfAR Krim Fellow Dr. Amy Chung and colleagues shed new light on this topic by highlighting the role of neutrophils, a more numerous and much more difficult cell to study, and their less well studied role in killing infected cells via antibodies.
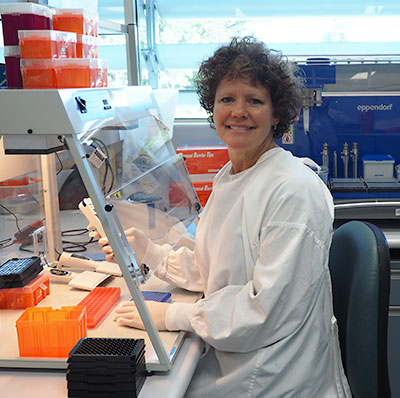
Unlike NK cells, which can persist for years, neutrophils live less than a week inside the body. Outside of the body, they die easily within a few hours and react so quickly to their new environment that, in a petri dish, they no longer resemble the cells the researchers set out to study. While it is known that neutrophils use antibodies to direct their killing ability towards HIV-infected cells, the mechanisms through which they do so remain a mystery.
A neutrophil
To spur this research, Dr. Chung developed a tool to study how antibodies in a patient’s blood might team up with neutrophils. To get around studying the fragile neutrophils in healthy blood, Dr. Chung developed the tool using cells from a cancer patient who donated her cells to science. It was Robert Gallo, one of three scientists credited with discovering that HIV causes AIDS, who archived the cells in 1977. In a petri dish, these cancerous cells can live indefinitely and maintain many of the same characteristics as fresh neutrophils.
Using this tool, Dr. Chung found, surprisingly, that neutrophils were six times better able than NK cells to kill HIV-infected cells when antibodies were present. The authors note that “neutrophil-mediated effector responses should be investigated in future HIV vaccine trials.”
Given what the field is learning about the diverse activities of antibodies (see here and here, for example), there is real potential for neutrophil function to also play an important role in an HIV cure.
Dr. Flores is amfAR’s associate director of research.